Let’s Talk About Breast Calcifications: Worry or Not?
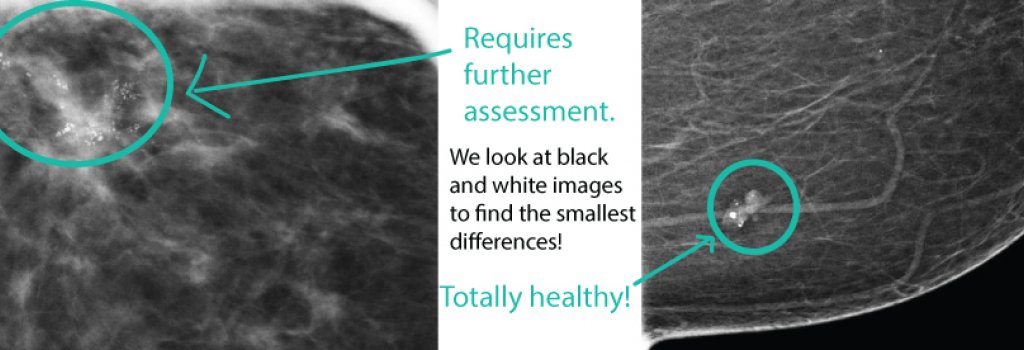
(Image: On the left is an example of microcalcifications that turned out to be a mix of invasive cancer and DCIS – notice how they branch out like tree limbs. On the right is an example of a fibroadenoma with chunky “popcorn-like” calcifications in the breast tissue.)
Breast calcifications are common and most often not a cause for concern. However, there are some calcifications in the breast that might prompt further evaluation. We as breast imaging doctors know that the need for further workup is a cause of anxiety. We hope to relieve some of that anxiety by discussing breast calcifications in detail.
Calcifications or small deposits of calcium in the breast can be seen for lots of different reasons and are something that can only be seen on imaging – nothing will be felt in the breast. Many calcifications radiologists can identify as non-cancerous or benign just by looking at their shape, size and distribution (or how they are situated in the breast tissue).
Calcifications of all types will appear as bright white on the mammogram. Knowing that the calcifications have been present on prior mammograms is helpful, so another reason we want those comparison studies! Occasionally, these benign type calcifications may not be quite so obvious or might be new. This could prompt additional mammographic imaging.
Benign type calcifications in the breast include the following:
- Vascular – calcifications in the walls of arteries may be seen in the breast; if you are less than 60 years of age, finding these may be a sign to look for other vessel disease (including hardening of the arteries in the heart, for example) but are common after the age of 60 and usually of no concern; may be better seen on 3D imaging;
- Skin – little punctate calcium deposits in the skin are quite common and usually easy to call normal findings; these are especially well seen on 3D studies;
- Calcifications in areas of prior breast trauma or surgery – these may pop up in areas where a small amount of breast fat dies – this can happen from injuries like seatbelt injuries and are commonly seen after breast reduction or other breast surgeries; if new, may need to be looked at more closely or followed at 6 months;
- Secretory or ductal calcifications – these may be described in the mammogram report as rod-like calcifications; these are benign and related to ductal secretions;
- Calcifications in some benign, non-cancerous growths in the breast, often fibroadenomas; these calcifications may look like popcorn – and when classic will not be a cause for concern; when early or a change, may require additional work up and/or 6 month follow up;
Breast calcifications can also be a sign of early breast cancer, a reason we radiologists pay close attention to all calcifications in the breast. The calcifications associated with breast cancer are usually quite small, often described as microcalcifications.
If microcalcifications are found on your mammogram, the radiologist will do the following to help determine what if anything needs to be done:
- Look at your old studies, if available. If these are new or this is a first time mammogram, further assessment may be needed.
- If further assessment is warranted on your screening mammogram, a diagnostic mammogram will be the next step in most cases, consisting of special magnification views that let us look up close at the calcifications. We will look at:
- The number of microcalcifications present;
- How the microcalcifications are distributed in the breast tissue with linear or branching distribution of the most concern;
- The shape of the individual calcifications with linear (thin line), branching or fine dust like shape worrisome features;
- The density or how white or grey the calcifications are with varying density a worrisome finding;
After reviewing the diagnostic magnification views, the radiologist will then decide:
- If classic for benign, non-cancerous calcifications, you can return to routine annual mammograms.
- If the calcifications cannot be determined to be benign, the next step may be to recommend biopsy. This is where a sample of the calcifications is removed from the breast tissue, often with a needle using mammograms as a guide. The tissue is then sent to a pathologist for review.
- Remember, even when the next step recommended is biopsy, this does not mean the calcifications are breast cancer – many patients who undergo biopsy for microcalcifications will end up with benign results. When microcalcifications are found in breast cancer, this can be from ductal carcinoma in situ (DCIS or stage 0 breast cancer) or occasionally from invasive cancers;
- On some occasions, the calcifications are thought most likely to be benign, but might warrant short term 6 month follow up mammograms.
In summary, calcifications are a common finding on mammograms. If your screening mammogram finds calcifications that warrant further evaluation, fear not. Most often, these will be found to be benign or noncancerous, even when we have to go to biopsy to find out for sure.





